Diffusion magnetic resonance imaging — which measures the random motion of water molecules in tissues — detected neurological degeneration in people with adrenoleukodystrophy (ALD), even when they did not show disease symptoms, a study reports.
That demonstrates the potential of this technique as a measure of disease progression, the researchers said.
The study, “Longitudinal diffusion MRI as surrogate outcome measure for myelopathy in adrenoleukodystrophy,” was published in the journal Neurology.
ALD is a rare genetic brain disorder caused by mutations in the ABCD1 gene that lead to the buildup of fatty molecules. That buildup causes nerve cell damage in the spinal cord — called myelopathy — and in the brain.
Clinical trials to test potential ALD therapies are limited by the lack of techniques that can accurately measure and quantify the disease’s progression. That makes it difficult to choose suitable outcomes to assess.
Health care providers currently use an array of clinical trial assessments. These include the Expanded Disability Status Scale or EDSS, to measure disability; the Severity Scoring System for Progressive Myelopathy (SSPROM), which evaluates the severity of myelopathy; the Timed Up-and-Go test, or TUG — which assesses the time needed to get up from an armchair and walk 6 meters, turning once; and the 6-Minute Walk Test (6MWT), to evaluate the maximum walking distance in 6 minutes.
However, a previous study showed that, while these assessments were able to detect disease progression after a two-year follow-up, the changes were small. That made it difficult to properly evaluate the effectiveness of a potential ALD therapy.
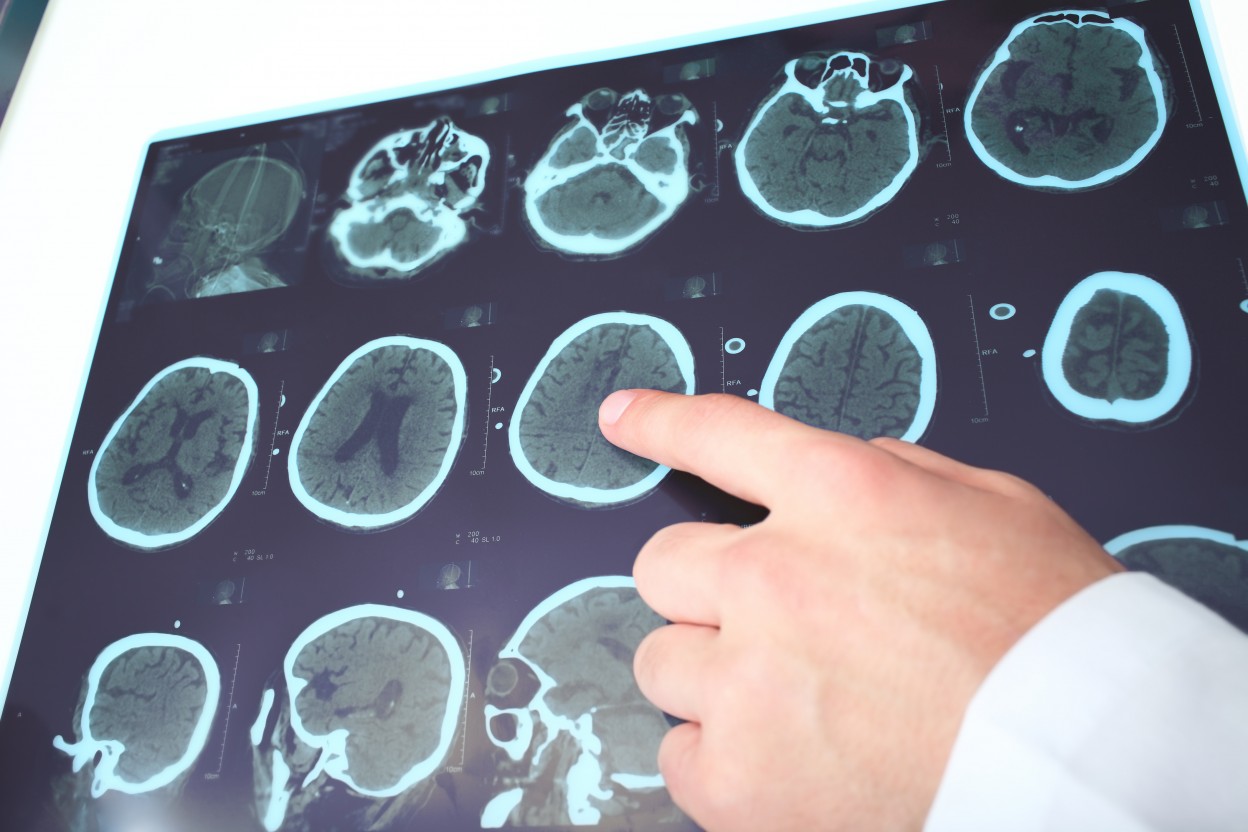
In an effort to find more accurate tools, the same team of researchers — from the University of Amsterdam, in the Netherlands — evaluated an imaging technique called diffusion magnetic resonance imaging (dMRI). Their goal was to determine if dMRI was an accurate measure of ALD progression.
dMRI is a non-invasive imaging technique that detects and measures changes in the random flow, or diffusion, of water in tissues, including the brain, where changes can be associated with nerve cell degeneration.
The team recruited a group of men with ALD and healthy controls at the Amsterdam University Medical Center between 2015 and 2018. In addition to the dMRI scans, participants were assessed using the standard clinical tests — EDSS, SSPROM, TUG, and 6MWT — at the start of the study, and at one- and two-years follow-up.
At the beginning of the study, brain scans were conducted on 52 ALD patients, ranging between ages 12 and 71, and 33 age-matched controls.
Following the publication of a 2016 study showing the utility of dMRI on the upper spinal cord (cervical) in ALD, the team added cervical spinal cord scanning to the study design. Upper spinal cord scans were available for 41 of the ALD patients, and 32 controls.
The diffusion MRI scans of people with ALD showed significant changes in water diffusion in the spinal cord and brain compared with controls, indicating nerve cell degeneration.
Significant differences were identified between control subjects and patients who showed symptoms (symptomatic), as well as those who did not show symptoms (asymptomatic). Further, the symptomatic group and the asymptomatic group also had measurable differences between them.
Moderate-to-strong correlations were identified between the brain and spinal cord dMRI calculations and all of the clinical measurements assessed. The strongest link was found between the spinal cord scan and the TUG test.
The analysis after the two-year follow-up showed significant changes in EDSS, SSPROM, and TUG clinical scores. Changes in the dMRI brain scans also were seen. However, the clinical changes did not correlate with the diffusion MRI measurements.
Interestingly, the brain dMRI scans detected changes in asymptomatic patients that were not identified using the clinical measurements, suggesting that dMRI may be more sensitive at detecting early ALD progression than the standard clinical tests.
“Our study illustrates the potential of dMRI as a surrogate outcome measure for myelopathy in men with adrenoleukodystrophy,” the researchers said. “As our follow-up time increases, we expect to show good longitudinal [over time] correlation with conventional clinical outcome measures in future studies.”