Robust donor cell transplant is needed for a successful repair of the blood-brain barrier in patients with cerebral adrenoleukodystrophy (cALD), a recent study suggests.
The study “Successful donor engraftment and repair of the blood brain barrier in cerebral adrenoleukodystrophy” was published in the journal Blood.
Up to 40 percent of boys affected by adrenoleukodystrophy develop the severe cALD form of the disease, which is associated with demyelination — loss of the protective myelin sheath surrounding neurons.
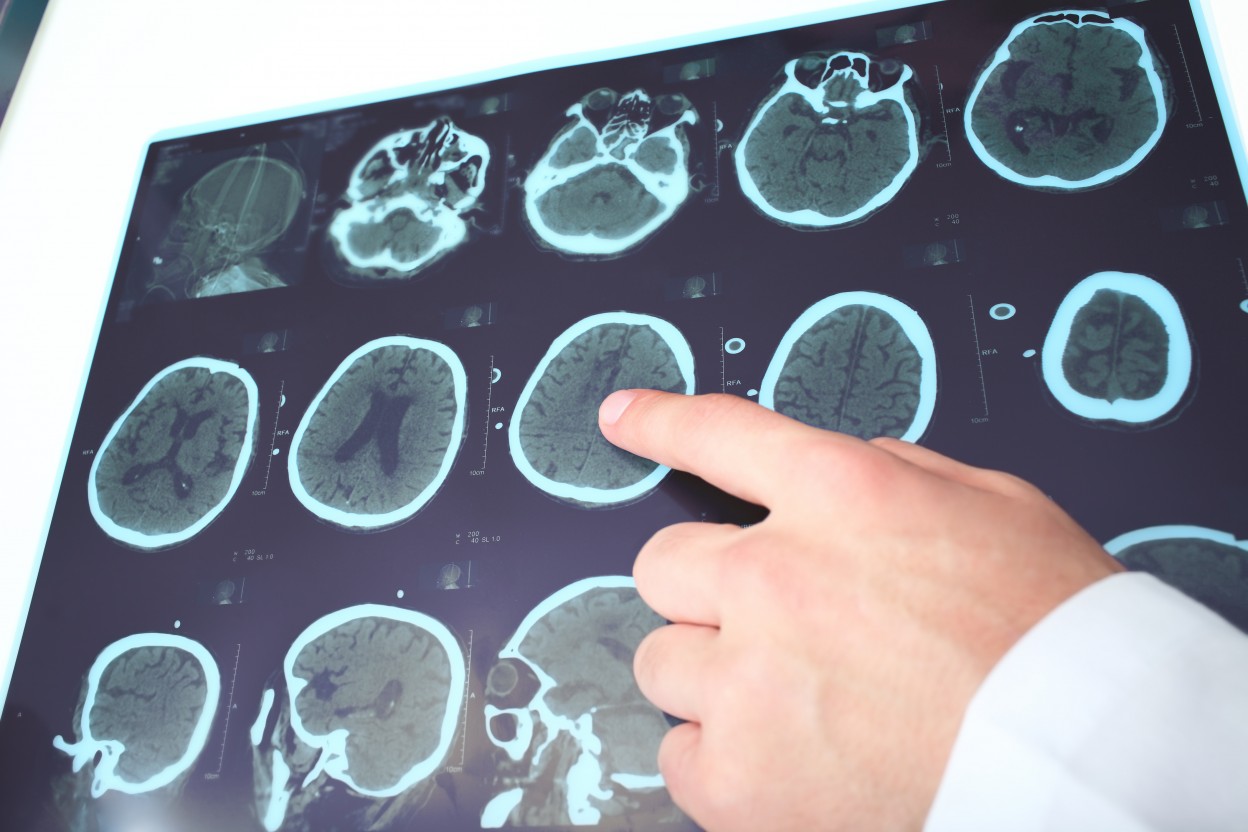
Demyelination can be seen through magnetic resonance imaging (MRI), based on the intensity of gadolinium in specific areas of the brain. Gadolinium is a chemical that accumulates in abnormal tissues after intravenous injection, and can be visualized by MRI.
Gadolinium-intense areas in the brain suggest active inflammation and a disrupted blood-brain barrier.
According to the research team, “only hematopoietic cell transplant (HCT) has been shown to halt neurologic progression with the best outcomes when HCT is performed early in the disease process, though the mechanism of disease arrest by donor hematopoietic cells is unknown.”
In HCT, patients receive an intravenous infusion of hematopoietic stem and progenitor cells from a healthy donor. The procedure is used to re-establish the patient’s immune system.
In order to assess gadolinium resolution in MRI — indicative of elimination of active neuroinflammation — and other potential biomarkers, researchers analyzed boys with cALD who had received HCT.
Specifically, the team investigated the relationship between donor cell recovery and intensity changes on gadolinium, and also assessed if gadolinium intensity reductions were associated with specific biomarkers.
The team evaluated 66 boys with cALD (median age of 8.3 years) who had undergone a successful HCT between December 2002 and April 2017. MRI before HCT assessed the disease status, while MRI after HCT (at days 30, 60, 100, 180, and 365) showed the relative changes in gadolinium.
A successful HCT is characterized by long-term neutrophil recovery. Neutrophils are a type of white blood cells that form an essential part of the body’s innate immune system.
When measuring neutrophil immune cell recovery in patients, the team found that the median recovery time was 16 days. Patients showing faster recovery rates, were more likely to show gadolinium reduction.
Also, increased recovery of total neutrophil counts was associated with an increase in immune cell counts and CD34, a marker for hematopoietic stem or progenitor cells.
Another marker associated with reduced gadolinium was CD15 (a marker of white blood cells called granulocytes). According to MRI results, increased donor chimerism — the percentage of post-transplant hematopoietic cells in the patient that are all of donor origin — of CD15 (70-100%) was associated with reduced gadolinium intensity.
In contrast, HCT graft failure was associated with poor gadolinium reduction.
Next, researchers analyzed biomarkers that could reflect the severity of cerebral disease in cALD. They found that a higher gadolinium score before HCT had a significant inverse association with gadolinium reduction 60 days after HCT. That means patients with more active inflammation had a lower gadolinium resolution 60 days after HCT.
The team also confirmed a significant association between the day of absolute neutrophil count recovery, and reduced gadolinium 60 days after HCT.
“These results demonstrate for the first time a correlation between donor cell recovery and recovery of the BBB [blood-brain-barrier] as indicated by the resolution of gadolinium enhancement on MRI,” the researchers wrote.
“Our data suggest that robust donor myeloid recovery is necessary for timely repair of the blood-brain-barrier,” they concluded.
Still, the mechanism behind stabilized cerebral disease through HCT remains unknown. Based on previous research, the team suggested that, upon HCT, certain immature immune cells may cross the blood-brain barrier, maturate, and subsequently help to reduce inflammation in the central nervous system. However, further studies are needed to confirm that hypothesis.