The success of blood stem cell transplants in boys with childhood cerebral X-linked adrenoleukodystrophy (CCALD) is influenced by the severity of white matter loss in the brain and the stem cells’ source.
Specifically, CCALD patients who had a severe loss of white matter and received a transplant from a matched donor outside their family were more prone to disease progression and major functional disabilities after the transplant.
The study, “Potential Risks to Stable Long-term Outcome of Allogeneic Hematopoietic Stem Cell Transplantation for Children With Cerebral X-linked Adrenoleukodystrophy” was published in the journal JAMA Neurology.
CCALD is a variant of X-linked ALD that affects children, mainly boys (around 70 percent), and is characterized by severe loss of white matter (which makes up the brain and spinal cord tissue in the central nervous system) leading to a rapid loss of cognitive function and adrenal insufficiency (when the adrenal glands fail to produce the necessary amount of steroid hormones, mainly cortisol).
Allogeneic (from a donor) hematopoietic (blood-forming) stem cell transplant, or HSCT, is an established therapeutic strategy for CCALD. The long-term benefits are thought to be mediated by donor-derived replacement of mainly microglial cells, the immune cells of the central nervous system.
However, the risk factors associated with stable neurocognitive survival after HSCT remain poorly studied.
To address this question, researchers in Germany performed a retrospective review of treatments and outcomes in a group of 36 boys (mean age 7.2 years) with CCALD who underwent HSCT at Charité Universitätsmedizin Berlin between 1997 and 2014.
Eighteen patients were symptomatic, showing clinical symptoms of adrenal insufficiency, while the other 18 did not show CCALD symptoms (pre-symptomatic patients).
The team reviewed the patients’ clinical data, including their scores in the ALD-disability rating score (range from 0-4), and their neurological function scores (range from 0-25).
“For all of these tools, a score of 0 indicates no abnormalities, whereas increasing numbers indicate worsening patient status,” researchers said.
Nine patients (25%) received a bone marrow transplant from a family member (in the majority of the cases a sibling), while the other 27 patients (75%) received stem cells from a matched, unrelated donor — 17 received bone marrow stem cells, nine received blood stem cells, and one received cord blood stem cells.
Results showed that after a median follow-up of 108 months, 75% of the patients (27 of 36) were alive, with an overall five-year survival rate of 81%.
All patients who received a bone marrow transplant from a matched family donor survived, while the 10-year survival rate of those who received a transplant from a matched unrelated donor was 68%.
When analyzing patient outcomes according to clinical data at the beginning of the study, researchers saw that 89% of the pre-symptomatic patients and 61% of those already showing clinical symptoms survived.
Moreover, 72% of the pre-symptomatic patients (13 patients) had an event-free survival, while only one patient (6%) among the symptomatic had an event-free survival. Each group had a median survival time of 49 and nine months respectively.
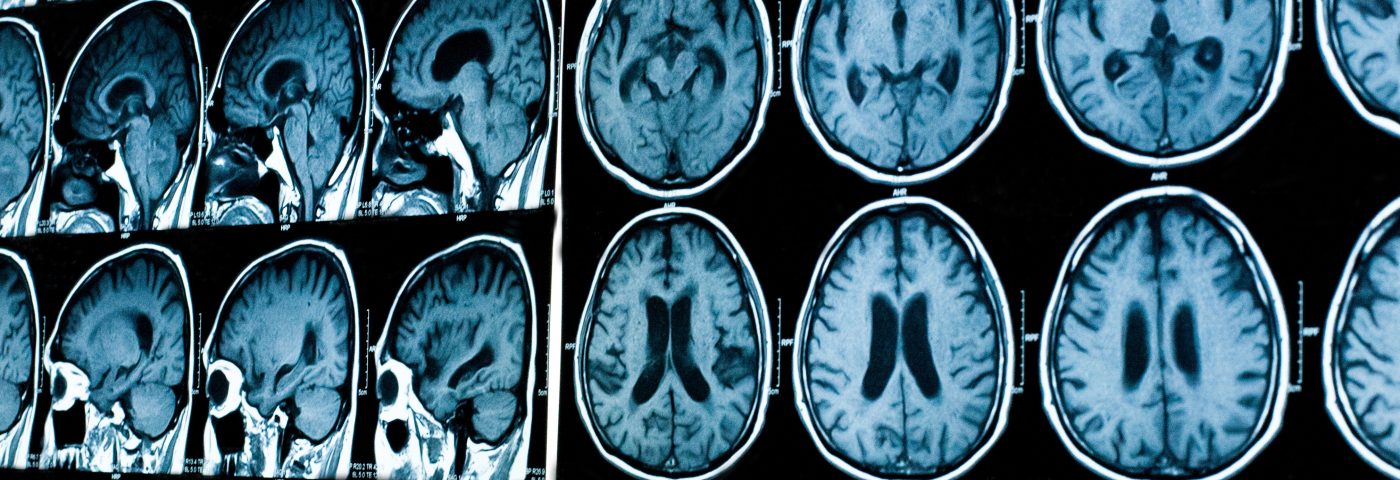
Researchers also analyzed patients’ brains through magnetic resonance imaging (MRI) before the transplant, and how they related to outcomes. Specifically, the team reviewed the severity of white brain matter loss, quantified through the Loes MRI severity score (ranging from 0-34, with higher scores meaning more severe losses).
Half the patients analyzed (18) were categorized as having a favorable MRI result, meaning a less severe loss of white matter before the transplant.
Results showed that none of these 18 patients died of progressive disease or developed major functional disabilities. Their event-free survival was 77%.
In contrast, the other 18 patients with higher Loes MRI scores showed extensive white matter loss. Of these, 13 patients developed epilepsy, and 10 developed major functional disabilities. Moreover, no patient in this group had an event-free survival.
Based on the white matter loss pattern and stem cell source, researchers divided participants into four groups according to event-free survival and major functional disability-free survival. This categorization showed that patients with a favorable MRI pattern and who received bone marrow from a matched donor had an event-free-survival of 100%, while those who received peripheral blood stem cells or cord blood had a major functional disability-free survival and event-free-survival of 71% and 43%, respectively.
Among those with an unfavorable MRI pattern — those whose loss of white brain matter affected two brain regions that play a major role in movement (the cerebellum and basal ganglia) — died because of major functional disabilities (four patients). Of the remaining patients within the unfavorable MRI group, half survived without major functional disabilities, but none had an event-free survival.
“This single-center case series found that all patients with favorable neuroimaging and matched bone marrow transplant had stable neurocognitive survival. In contrast, the disease progressed for all patients without these factors, and many developed major functional disabilities,” the researchers said.
“Newborn screening for the disease and regular neuroimaging are recommended, and patients who lack a matched bone marrow donor may need to find new therapeutic options,” the team concluded.